Unstable Angina
Angina is a feeling of pain, tightness, pressure, or discomfort in and around your chest. It can occur if your heart muscle isn’t getting enough oxygen-rich blood. There are 2 types of angina. They are stable and unstable.
Stable angina occurs at times you can predict. It is constant in how long it lasts and how intense it is. This might be during or after exercise or when you exert yourself. This type of angina can often be managed with medicine or rest.
Unstable angina does not occur at times you can predict. It can be more intense and last longer. And it may not respond to the usual forms of treatment. It's a warning that a heart attack (acute myocardial infarction) is possible in the near future. For this reason, it should be treated right away.
If you have questions, be sure to ask your health care provider.
Coronary disease causes angina
Your heart is a muscle. It gets oxygen from the blood sent through the coronary arteries.
Coronary artery disease (CAD) occurs when fatty material (plaque) builds up within your artery walls. Plaque irritates and inflames the artery wall. The buildup of plaque can reduce blood flow to your heart. This reduces the amount of oxygen your heart gets. The lower amount of oxygen can cause the chest pain of angina.
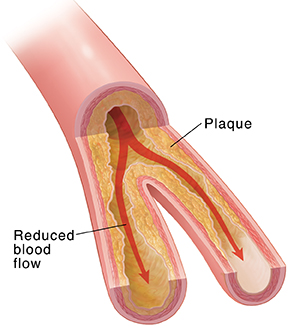 |
| Unstable angina is usually caused by coronary artery disease (CAD). |
Other symptoms of angina include feeling lightheaded, shortness of breath, nausea, belly pain, heart palpitations, and sweating for no clear reason.
The difference between stable and unstable angina
-
Stable angina. This type of angina occurs most often during exercise or times of stress. Stable means that this type of angina is consistent and predictable. Stable angina goes away when you rest or take nitroglycerin. This is a medicine that allows the heart muscle to relax. It helps increase blood flow through your arteries.
-
Unstable angina. Unstable angina is described as chest pain that occurs without warning, even when you rest. You may also be told you have unstable angina if you have stable angina that becomes more severe, lasts longer, or that is not relieved by rest or medicine.
How unstable angina feels
Unstable and stable angina have the same symptoms. With unstable angina, the symptoms are more severe and last longer. Symptoms include:
-
Discomfort, aching, heaviness, tightness, squeezing, or pressure. You may feel this in your chest or back. You may also feel it in your arm, shoulder, neck, jaw, or upper belly.
-
Feeling more tired than usual for no clear reason.
-
Feeling lightheaded.
-
Nausea.
-
Sweating for no clear reason.
-
Shortness of breath.
-
Heart palpitations.
Not everyone who has a heart attack has the typical symptom of chest pain. You may be having a "silent" (unrecognized) heart attack if you lose consciousness (syncope), or you have confusion, weakness, or changes in thinking (delirium).
Get medical help right away to find out if you are having a heart attack or another serious condition.
Your evaluation
Because unstable angina can lead to a heart attack, it is viewed as an emergency. If you are having symptoms of unstable angina, you should call 911 right away. Your health care provider will ask about your symptoms and examine you. Tests will be done quickly. Common tests include:
-
Blood tests.These can help tell if there is damage to your heart. They may be repeated often, usually every 6 to 8 hours until you have 3 sets. They can also check for cholesterol in the blood, which leads to plaque buildup. They can check for other health problems that affect the heart, such as diabetes.
-
Electrocardiogram (ECG). This test records your heart’s electrical patterns. A resting ECG can show if you have damage to your heart muscle or a change in the way your heart beats. It's the quickest way to diagnose an acute heart attack. But not every heart attack is found by an ECG. Once your symptoms are more stable, a stress ECG (stress test) can show how well the blood flows to your heart while you exercise or when a medicine is given to you.
-
Angiography. This test can show where your arteries are narrowed. The health care provider puts a long tube (catheter) in an artery in your arm, neck, or leg (groin). They slowly guide it to your heart. Contrast material is sent through the tube and into the coronary arteries. This makes the arteries show up clearly on X-rays. This helps show any blockages or areas where plaques have narrowed the artery.
Treating unstable angina
Your treatment will depend on the results of your tests. Possible treatments include:
-
Observation. If your symptoms are severe, you may need to stay in the hospital. If your chest pain gets better, the tests show no sign of damage to your heart, and your stress test shows you are at low risk for a future heart attack, you may be able to go home.
-
Medicines. Your health care provider will likely give you nitroglycerin. You also may be given medicines that help prevent blood clots, such as aspirin. And you may be given medicines to help reduce your blood pressure or slow your heart rate.
-
Procedures to improve blood flow. If your chest pain doesn't get better, your health care provider may suggest procedures to improve blood flow to your heart muscle. These can include angioplasty with a stent or bypass surgery. Your provider will tell you more about these treatments if you need them.
-
Lifestyle changes. Lifestyle changes usually include not smoking, eating healthy foods, losing weight, and getting regular exercise. These changes will take time to reduce your risk of having a heart attack. For them to work, you will need to do them for the long term. The sooner you start, the better it will be for your overall health.
If you have other health problems, such as high blood pressure, diabetes, or high cholesterol, these need to be treated as well. They can increase your risk for a heart attack. Lifestyle changes can make unstable angina attacks less frequent and less severe. Staying away from alcohol and stimulants can reduce the stress on your heart as well. They also help you manage CAD and reduce your risk for a heart attack.
When taking nitroglycerin
If your health care provider prescribes nitroglycerin, be sure to follow their instructions on how to use it. Also be sure to tell your provider if you’re taking any other medicines. This includes other prescription and over-the-counter medicines, as well as herbs and other supplements. Talk to your health care provider before you take nitroglycerin if you take medicines to treat erectile dysfunction or pulmonary hypertension. These can include sildenafil, tadalafil, or vardenafil. Taking these medicines together can cause a dangerous drop in blood pressure.
When to call 911
Call 911 or go to the emergency room (ER) right away if your chest pain:
-
Occurs when you’re not active.
-
Wakes you up from sleep.
-
Comes back and is not relieved by your usual dose of nitroglycerin.
-
Occurs with weakness, dizziness, fainting, heavy sweating, nausea, or vomiting.
-
Lasts longer than 5 minutes.
-
Feels like it's getting worse.