When Your Child Has an Elimination Dysfunction
Children often develop an elimination dysfunction during or after they are potty-trained. Your child’s doctor will talk to you about options for treatment.
What is an elimination dysfunction?
It's a problem holding or releasing urine or stool. Infants release (eliminate) urine or stool by reflex. As a child gets older, they learn to control these functions. A child may have a problem learning this control. This is called an elimination dysfunction. These children may be prone to urinary accidents during the day (diurnal enuresis) or night (nocturnal enuresis), bowel accidents (encopresis), or urinary tract infections (UTIs).
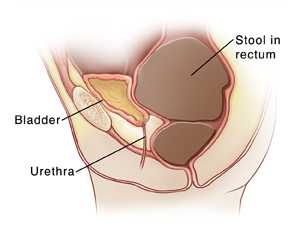 |
| Constipation can lead to wetting accidents when a too-full rectum pushes against the bladder. |
What causes an elimination dysfunction?
In most cases, this problem occurs because a child holds in urine or stool for too long. Children may put off using the bathroom because they don’t want to stop playing. This puts them at risk for wetting or soiling events. It can also lead to the inability to release stool (constipation). Other causes include:
-
Neurodevelopmental disorders.
-
Delayed bladder maturation.
-
Spinal cord trauma or tumor.
-
Muscle disorders affecting the pelvic floor.
-
Emotional causes.
What are the signs?
Signs of an elimination dysfunction include:
-
Involuntary release of urine (incontinence) during the day or nighttime.
-
Constipation.
-
Problems with urine flow, such as trouble starting or weak flow.
-
Infrequent or frequent release of urine (voiding).
-
Painful urination.
-
Urinary tract infection.
-
Low-back, belly (abdominal), or side (flank) pain.
-
Liquid poop leakage onto the underwear.
-
Poop leakage with the passing of gas.
-
No feeling of having to pass poop before leakage happens.
How is an elimination dysfunction diagnosed?
Your child’s doctor will ask you about your child’s health. A physical exam will also be done to look for problems. To help learn more:
-
You may be asked to keep a record of your child’s bathroom habits.
-
A kidney ultrasound may be done. This checks for blockages in the urinary tract and swelling of the kidneys.
-
A urodynamics study may be done. This tells your child's doctor how your child’s bladder and urethra work.
-
An anorectal manometry may be done. This test studies the nerves and muscles of the anus and rectum by measuring pressure and sensation. It can help diagnose when there is a spinal cord injury or local injuries in the sphincter muscles. This test also helps diagnose a condition called Hirschsprung disease. This condition causes blockage in the large intestine.
-
A barium enema may be done. This is a type of X-ray to check the lower gastrointestinal tract. The doctor gently inserts a well-lubricated tube (enema tube) into your child's rectum and slowly fills it with barium sulfate. The barium flows into your child's colon and coats the lining of the lower GI tract, making it visible on X-ray. The doctor monitors the flow of the barium on an X-ray screen to assess areas of narrowing (anal atresia).
How is an elimination dysfunction treated?
Treatment depends on the cause, type, and severity of the problem. Your child may need one or more types of treatment. Common treatments include:
-
Behavioral therapy. This helps your child change their bathroom patterns. It may also include:
-
Biofeedback therapy. This helps your child locate the muscles used to control the release of stool or urine. They can learn to relax them at the right time.
-
Medicine. This can help relax the bladder, if needed. Oral laxatives, suppositories, or enemas may be given to relieve constipation. Changes in diet, bowel training, and laxatives may also be used.
-
Dietary modifications. The doctor may make changes to your child's diet. This may include adding more fiber. Fiber helps poop retain water and prevent constipation. Your child may need to drink more water and get regular exercise.
-
Intermittent catheterization. This procedure drains the bladder on a regular schedule. A tube (catheter) is put into the urethra and into the bladder. This is done each time the bladder needs to be emptied. This treatment is mainly used in severe cases.
Timed voiding and bowl retraining
Timed voiding means urinating at set times. It lets kids who are potty-trained empty their bladders on a regular basis. This helps prevent infections. It also helps to avoid wetting accidents. Your child will need to visit the bathroom at set times throughout the day. Their doctor can suggest how often your child should urinate. When practicing timed voiding, your child should not wait until the urge to urinate arises before using the toilet.
Bowel retraining is a process can help your child have normal poop (bowel movements). Your child sits on the toilet for a short time after meals. This helps the body reconnect eating with having bowel movements. Your child's doctor will talk with you about the best way to start bowel retraining.
Coping with an elimination dysfunction
This problem can be frustrating for children and families. Be supportive and patient. It takes work and time to create new bathroom habits. Encourage your child’s success. In some cases, a therapist can help kids and their families follow the treatment plan.